Corneal Wound Healing
Corneal abrasion is one of the most common ocular injuries and is the leading eye-related condition seen in emergency departments. Damage to the corneal surface can lead to inflammation, loss of epithelial integrity, and in some cases, abnormal blood vessel growth into the cornea (neovascularization).
Model Overview
Injury to the corneal surface triggers a wound healing response that may include epithelial cell migration, stromal remodeling, and angiogenesis. EyeCRO offers multiple approaches for inducing these responses, including an alkali burn model and a mechanical injury model, allowing flexibility to match study design and therapeutic targets.
Progress is monitored by slit-lamp imaging and histologic analysis. Quantitative assessment of neovascular area, opacity, and wound closure provides reproducible, objective measures for comparing treatments.
These models are used to evaluate anti-angiogenic therapies, wound healing agents, and interventions that aim to restore corneal clarity and prevent vision loss.
Typical Endpoints
- Corneal opacity scoring over time
- Quantification of neovascular area and vessel length
- Epithelial defect closure rate (fluorescein staining)
- Vessel growth and regression timelines
- Histologic or imaging analysis of corneal tissue
Representative Data
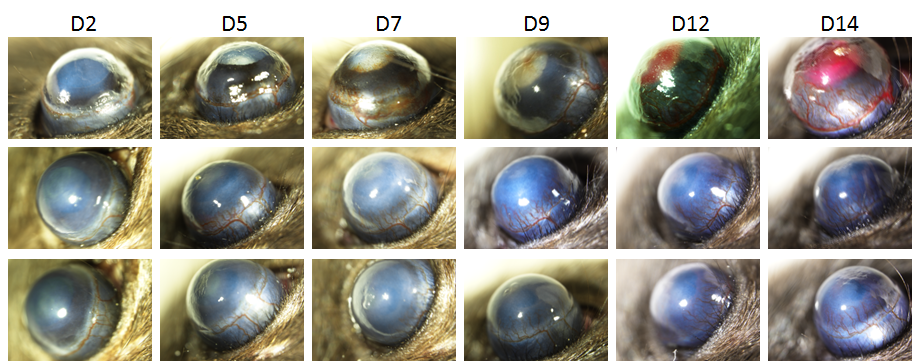
Top: Slit-lamp imaging from Day 2 to Day 14 shows increasing corneal opacity and vessel ingrowth after injury
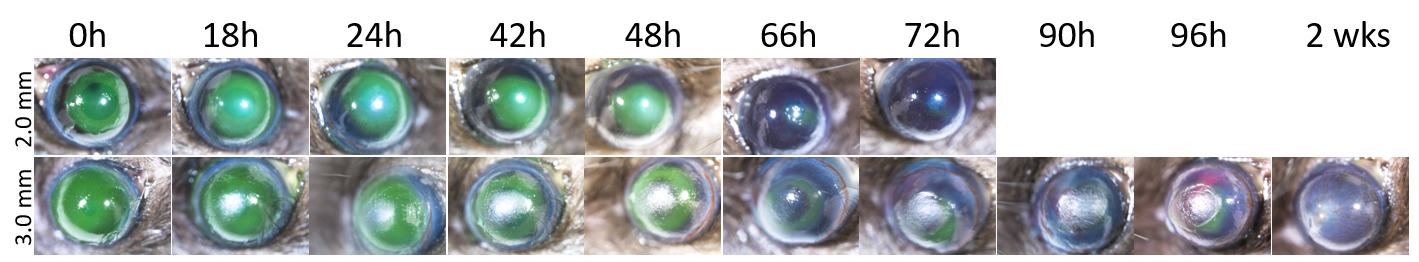
Middle: Fluorescein-stained images from 0 hours to 2 weeks demonstrate progressive wound closure for 2.00 mm and 3.00 mm wounds
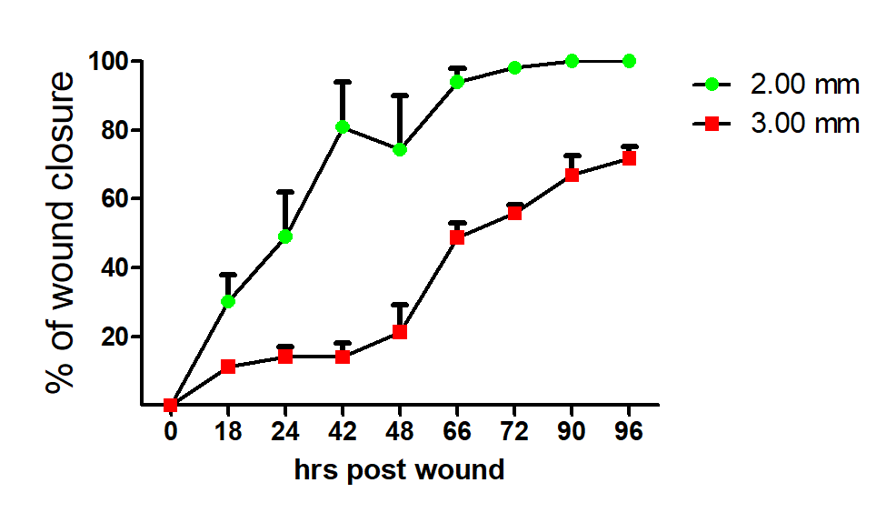
Bottom: Graph showing percentage of corneal wound closure over time, with faster healing in 2.00 mm wounds compared to 3.00 mm wounds
Interested in this model?
We are happy to share more about study design options, endpoints, or timelines.
Contact us to discuss your study goals.
