Allergic Conjunctivitis
Ocular allergic disease is marked by inflammatory responses of the conjunctiva and affects approximately 15–20% of the population. These hypersensitivity reactions may be IgE-mediated, T-cell mediated, or involve both arms of the immune system.
Model Overview
Acute allergic conjunctivitis is driven by IgE-mediated mast cell degranulation, while chronic disease results from ongoing activation of mast cells and other inflammatory pathways. These responses affect the conjunctiva, cornea, and eyelids and may be acute or persistent.
In this model, mice are sensitized with short ragweed pollen (SRW) or ovalbumin (OVA) and subsequently challenged ocularly with the same antigen. This induces a reproducible allergic response mimicking key clinical features of human ocular allergy.
Typical Endpoints
- Clinical scoring: chemosis, conjunctival redness, lid edema, discharge, hyperemia
- Th2 cytokine expression in conjunctiva (qPCR, ELISA, multiplex)
- Histology: quantification of eosinophils, neutrophils, mast cells
- Systemic IgE levels
- Whole blood cell differentials
Representative Data
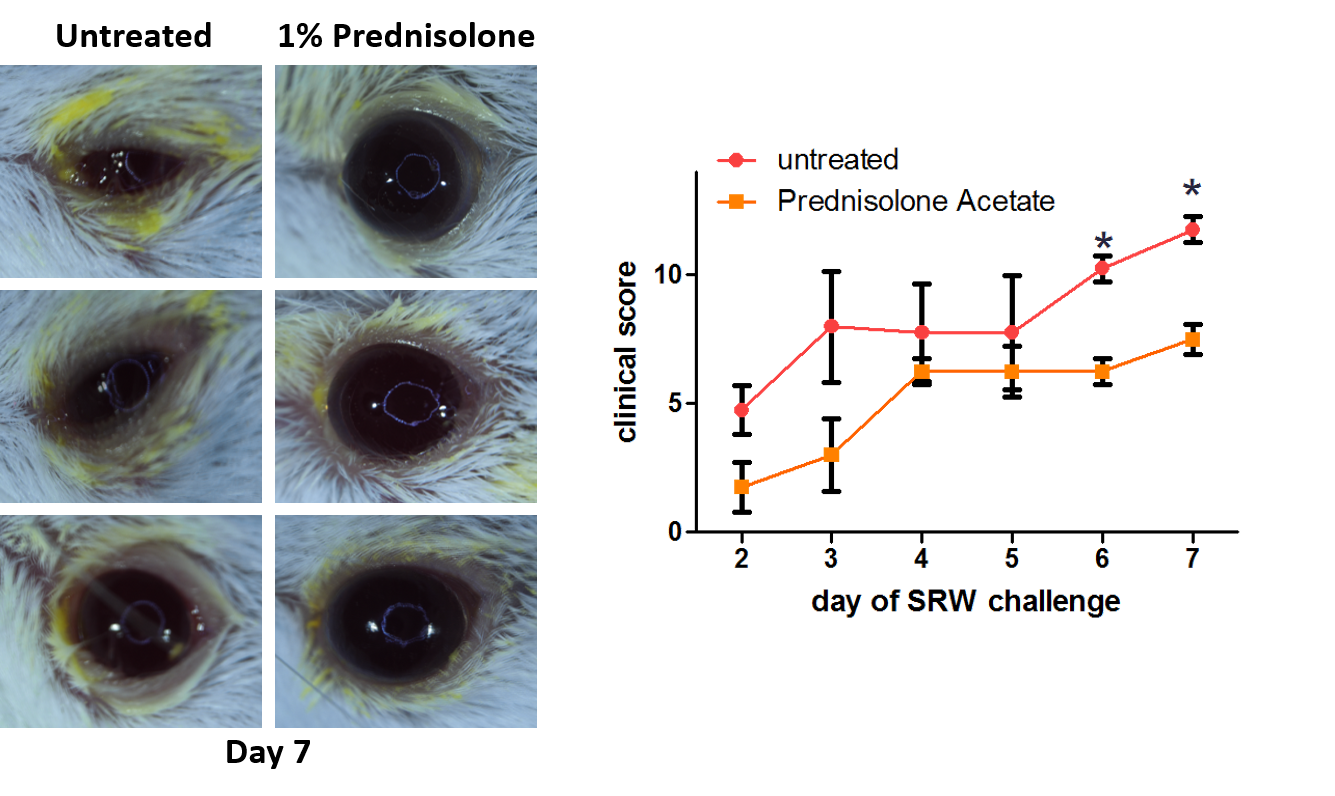
Left Column: Untreated animals display visible conjunctival redness, chemosis, and discharge following short ragweed pollen (SRW) challenge.
Right Column: Animals treated with Prednisolone Acetate show markedly reduced inflammatory signs.
Graph: Clinical scoring over 7 days demonstrates a consistent reduction in ocular inflammation in treated animals
Interested in this model?
We are happy to share more about study design options, endpoints, or timelines.
Contact us to discuss your study goals.
